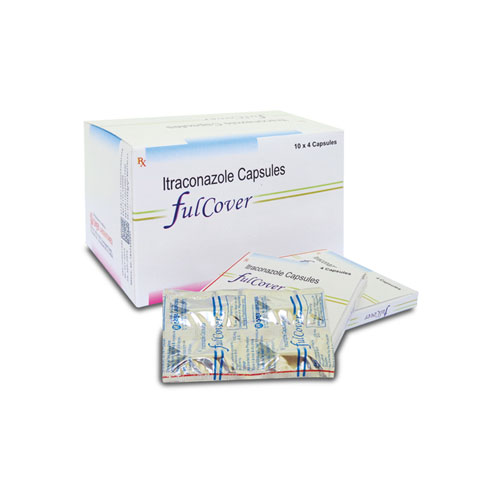
FULCOVER Capsule
Therapeutic Class
Antifungals
Indications
FULCOVER capsules are indicated for: Persistent vulvovaginal candidiasis which does not respond to conventional therapy. Dermatomycosis which does not respond to conventional therapy. Although proof of efficacy is limited, FULCOVER capsules have been used in fungal keratitis. Onychomycosis, caused by dermatophytes and/or yeasts and which does not respond to other therapy. Although proof of efficacy is limited, FULCOVER capsules have been used in: systemic aspergillosis and candidiasis, histoplasmosis, sporotrichosis, paracoccidioidomycosis and blastomycosis.
Chemical Composition
Each capsule contains:
Itraconazole Pellets
Equivalent to Itraconazole BP :100 mg
Excipients : Q.S.
Packaging
1 x 10 x 4's/ Box
Dosage & Administration
Oropharyngeal Candidiasis. Adult : 100 mg daily for 15 days Vulvovaginal candidiasis. Adult: 200 mg bid for 1 day. Pityriasis versicolor- Adult: 200 mg daily for 7 days. Tinea corporis and tinea cruris - Adult: 100 mg daily for 15 days or 200 mg daily for 7 days. Fungal nail infections -Adult: 200 mg daily for 3 month. Systemic fungal infections -Adult: 100-200 mg once daily, increased to 200 mg bid for invasive or disseminated infections. Primary or secondary prophylaxis of infections in neutropenic or AIDS patient. Adult: 200 mg daily increased to 200 mg bid if necessary. Tinea pedis or tinea manuum- Adult: 100 mg daily for 30 days or 200 mg bid for 7 days.
Contraindications
Itraconazole is contraindicated in: Hypersensitivity to itraconazole or to any of the capsule excipients. Pregnancy. However, itraconazole may be given if the fungal infection is life-threatening and the potential benefit is considered to outweigh the potential risk to the foetus. Adequate contraceptive precautions should be taken by women of childbearing potential using Itraconazole until the next menstrual period following the end of therapy. Patients taking terfenadine, astemizole, mizolastine, cisapride, dofetilide, quinidine, pimozide, CYP3A4 metabolised HMG-CoA reductase inhibitors such as simvastatin and lovastatin, triazolam and oral midazolam capsules.
Warning & Precautions
» There is no information regarding cross hypersensitivity between Itraconazole and other azole antifungal agents. Caution should be used in prescribing Itraconazole to patients with hypersensitivity to other azoles. » In a healthy volunteer study with intravenous Itraconazole, a transient asymptomatic decrease of the left ventricular ejection fraction was observed. » Itraconazole has been shown to have a negative inotropic effect and has been associated with reports of congestive heart failure. Itraconazole should not be used in patients with congestive heart failure or with a history of congestive heart failure unless the benefit clearly outweighs the risk. » Caution should be exercised when co-administering Itraconazole and calcium channel blockers. » Itraconazole has a potential for clinically important drug interactions. (See 4.5: Interaction with other medicaments and other forms of interaction). » Decreased gastricacidity: Absorption of Itraconazole is impaired when gastric acidity is decreased. In patients also receiving acid neutralising medicines (e.g. aluminium hydroxide) these should be administered at least 2 hours after the intake of Itraconazole Capsules. In patients with achlorhydria such as certain AIDS patients and patients on acid secretion suppressors (e.g. H2-antagonistsproton-pump inhibitors) it is advisable to administer Itraconazole Capsules with a cola beverage. » Hepatic impairment » Itraconazole is predominantly metabolised in the liver. A slight decrease in oral bioavailability in cirrhotic patients has been observed, although this was not of statistical significance. The terminal half-life was however significantly increased. The dose should be adapted if necessary. » Renal Impairment; The oral bioavailability of Itraconazole may be lower in patients with renal insufficiency. Dose adaptation may be considered.
Side Effects
Dyspepsia, abdominal pain, nausea, vomiting, diarrhoea, menstrual disorders, constipation, rash, pruritus, urticaria; angioedema, anaphylaxis. Increased liver enzyme values, jaundice, Stevens-Johnson syndrome, hypokalaemia.
Drug Interaction
Drugs affecting the metabolism of Itraconazole: (1) Interaction studies have been performed with rifampicin, rifabutin and phenytoin. Since the bioavailability of Itraconazole and hydroxyitraconazole was decreased in these studies to such an extent that efficacy may be considerably reduced, the combination of Itraconazole with these potent enzyme inducers is not recommended. No formal study data are available for other enzyme inducers, such as carbamazepine, phenobarbital and isoniazid, but similar effects should be anticipated. (2) Effects of Itraconazole on the metabolism of other drugs: Itraconazole can inhibit the metabolism of drugs that are substrates for cytochrome 3A isoenzymes. This can result in an increase and/or a prolongation of their effects, including side effects. After stopping treatment, Itraconazole plasma levels decline gradually, depending on the dose and duration of treatment. This should be taken into account when the inhibitory effect of Itraconazole on co-administered drugs is considered. Examples are: Drugs which must not be used during treatment with Itraconazole: Terfenadine, astemizole, mizolastine, cisapride, triazolam, oral midazolam, dofetilide, quinidine, pimozide, CYP3A4 metabolised HMG-CoA reductase inhibitors such as simvastatin and lovastatin. Caution should be exercised when co-administering Itraconazole with calcium channel blockers. In addition to possible pharmacokinetic interactions involving the drug metabolising enzyme CYP3A4, calcium channel blockers can have negative inotropic effects which may be additive to those of Itraconazole. If the following are co-administered with Itraconazole, their plasma levels, clinical effects and possible side effects should be monitored. The dose of these drugs may need to be reduced during co-administration with Itraconazole: » Oral anticoagulants : » HIV protease inhibitors such as ritonavir, indinavir, saquinavir » Certain antineoplastic agents such as vinca alkaloids, busulphan, docetaxel and trimetrexate » CYP3A4 metabolised calcium channel blockers such as dihydropyridines and verapamil » Certain immunosuppressive agents: cyclosporin, tacrolimus, sirolimus.

